– Simultaneous measurement of brachial pulse waveform and heart sound for easy measurement –
Researchers) SUGAWARA Jun, Group Leader, Human Informatics and Interaction Research Institute
- Developed a simple measurement technique to evaluate the aorta proximal stiffness, which is associated with the development of cardiovascular disease
- A simple measurement is used in the same way as upper arm blood pressure measurement, reducing the burden of testing.
- Detecting the proximal aortic stiffening, which starts in the 30s, may contribute to earlier and more sensitive identification of cardiovascular disease risk.
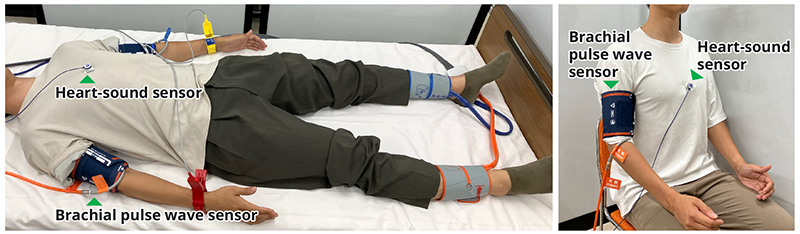
PWV measurement: The conventional method requires sensors on both arms and legs and measurement in the supine position (left), but this method requires only a heart-sound sensor and brachial pulse wave sensor, and measurement can be done in the sitting position (right).
Jun Sugawara, Leader of the Physiological System Research Group, at the Human Information Interaction Research Group, National Institute of Advanced Industrial Science and Technology (AIST), in collaboration with Professor Hiroshi Tomiyama and Senior Professor Akira Yamashina (at the time of the research) of the Department of Cardiovascular Medicine, Tokyo Medical University, and Professor Hirofumi Tanaka of the University of Texas at Austin (UT), U.S.A, have developed the pulse wave velocity (PWV; baPWV, hbPWV, and CAVI are also classified as PWV).
Cardiovascular disease (CVD) is a major cause of death and a significant healthcare burden in Japan. Measuring and evaluating arterial stiffness, a key contributing factor to CVD, can help prevent the onset of such diseases. Brachial-ankle pulse wave velocity (baPWV), a widely used systemic index of arterial stiffness in Japan and abroad, increases significantly after middle age (around the 50s). To measure baPWV, patients must lie down with blood pressure cuffs wrapped around their upper arms and ankles.
In contrast, heart-brachial pulse wave velocity (hbPWV), which was investigated for its usefulness in this study, reflects the stiffness of the proximal aorta. Since proximal aortic stiffness increases linearly with age, starting as early as the 30s, evaluating hbPWV may allow for earlier and more accurate detection of CVD risk than baPWV. Additionally, hbPWV, which is calculated from simultaneous measurements of heart sounds and brachial pulse waveforms, can be measured in a sitting position, similar to how brachial blood pressure is measured, thereby reducing the burden on both the patient and the healthcare professional.
The algorithm for hbPWV measurement could be integrated into spot arm sphygmomanometers and even home blood pressure monitors. This would increase the opportunities to measure arterial stiffness indices and provide more chances for early detection of CVD risk.
Details of this technology were published in Hypertension Research on August 1, 2024.
CVD is one of the leading causes of death in Japan and worldwide, with arterial stiffness being a key risk factor for its development. Arterial stiffness, which reflects the rigidity of the arterial walls, has gained attention as a valuable indicator of CVD risk.
Central large arteries, such as the aorta and carotid arteries, are highly elastic and function as cushions to absorb the blood flow ejected from the heart. However, as arteries lose their elasticity with age and their cushioning function diminishes, chronic stress on the heart increases, increasing the risk of CVD. Since arterial stiffness increases with age, it is crucial to detect this risk early by measuring it.
Journal: Hypertension Research
Title of paper: Cross-Sectional and Longitudinal Evaluation of Heart-to-Brachium Pulse Wave Velocity for Cardiovascular Disease Risk
Author: Sugawara J, Tanaka H, Yamashina A, Tomiyama H.
DOI: 10.1038/s41440-024-01805-5