- Towards regenerative medicine transplanting patient’s own stem cells to diseased parts -
Makoto Asashima (AIST Fellow), the National Institute of Advanced Industrial Science and Technology (AIST; President: Tamotsu Nomakuchi), Tomoko Kuwabara (Senior Researcher), Stem Cell Differentiation Research Team, and Yuzuru Ito (Leader) and Yasuko Onuma (Researcher), Organ Development Research Team, the Research Center for Stem Cell Engineering (Director: Makoto Asashima) of AIST, have developed an effective regenerative therapy method for diabetes on the basis of rat experiments in collaboration with Fred H. Gage (Professor), the Salk Institute for Biological Studies, USA. This method involves transplantation of adult neural stem cells into the pancreas. The therapeutic efficacy of this method has been confirmed.
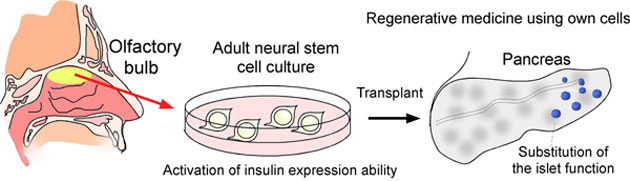
In the basic stage of this research, the researchers demonstrated that neurons have the intrinsic capacity to produce insulin as pancreatic cells have and elucidated the mechanism for activation of this capacity. Adult neural stem cell lines, which develop into neural cells, can be established and cultured not only by intracerebral collection, which requires difficult surgery, but also by collection from the olfactory bulb, which is relatively easy. It has been confirmed that, when adult neural stem cells are collected from diabetic rats, established as cultures, and transplanted into the pancreases of diabetic rats once a state of ready insulin production has been achieved, a decreased blood sugar level can be maintained. This technique has the potential for use in safer and more natural regenerative medicine using autologous cells without gene transfer.
Details of the results will be published in a European scientific journal, “EMBO Molecular Medicine.”
 |
|
Figure 1: Concept of regenerative therapy for diabetes using autologous cells |
The number of diabetes patients in Japan has increased markedly in recent years. If people with pre-diabetic conditions are included, the total number is estimated to be as high as 10 to 20 million. Numerous diabetes patients suffer increased severity after the onset, involving complications such as retinopathy and nephropathy, and an important issue is therefore the establishment of radical diabetes treatments.
Transplantation of pancreatic islets (islets of Langerhans) from the pancreas of a different donor is an effective treatment method for type-1 diabetes. However, because of the characteristics of the pancreas that contains large amounts of digestive enzymes, in order to obtain a pancreas that can be transplanted, the necessary preparation includes searching for a potential donor while still alive and ascertaining compatibility. As a result, the problem of shortage of donors for pancreatic islet transplantation is extremely serious. There are also other problems with this treatment method, including its high medical cost due to the need for concomitant post-transplantation administration of immunosuppressive agents and the decrease in metabolic activity due to the immunosuppressive agents. Stem cell transplantation can be used as an alternative to pancreatic islet transplantation, but an important issue is how efficiently and safely stem cells for use in transplantation can be prepared. Therefore, in order to achieve long-term stabilization of post-transplantation patients, there is a need for safer stem cells that have properties compatible with the pancreas into which they are transplanted and that can be used without operations such as gene transfer that might cause future carcinogenesis, etc.
AIST has been analyzing intracerebral neural stem cells and research has been carried out for use in development of medical treatments and drug discovery for Alzheimer’s disease and depression. In the course of this research, it was realized that the regulatory mechanism of adult neural stem cells are closely similar to that of the pancreatic cellular lineage. The mechanism was then analyzed in more detail, because these findings relate to techniques in which neural stem cells are used as substitutes for cells that function in the pancreas and offer the potential for use in regenerative therapy for diabetes and pancreatic disease. Cutting-edge research on adult neural stem cells has also been carried out at the Salk Institute for Biological Studies in the USA. Through collaboration with Professor Fred H. Gage of that Institute, the properties and capacities of these cells have been analyzed in detail using adult neural stem cells from the adult hippocampus and also from the olfactory bulb, from which cells can be collected more readily.
This research was supported by a Grant-in-Aid for Scientific Research (B; Grant-in-Aid for Young Scientists) of the Japan Society for the Promotion of Science and by Suzuken Memorial Foundation.
Neural stem cells, which are responsible for neurogenesis, are present in the adult brain. In recent years, it has been shown that neural stem cells are present in the adult olfactory bulb and give rise to neurogenesis. In addition, during basic research relating to adult neural stem cells, it was found that the genes required for insulin production are expressed in adults in both the pancreas and the cerebral nervous system. In terms of application to regenerative medicine involving collection of autologous cells and use of them as the cell source for transplantation, endoscopic collection of neural stem cells from the olfactory bulb is preferable to collection of intracerebral neural stem cells by means of difficult surgery.
Adult neural stem cells were collected from both the hippocampi and the olfactory bulbs of rats and cultured. Comparative analyses of gene expression were carried out using a micro-array method to investigate the expression of genes such as those essential for insulin production and those important for differentiation. The findings showed that the genes for insulin production are expressed during the process of differentiation to neurons in both neural stem cells derived from the hippocampus and those derived from the olfactory bulb.
Neural stem cell lines were established from both the hippocampi and the olfactory bulbs of diabetic rats and the results of transplantation were investigated. After culturing the neural stem cells for two weeks in cell culture solutions containing agents that promote insulin production, they were transplanted into the pancreases of diabetic rats. Blood sugar levels of the rats indicating their diabetic disease states were measured regularly and it was found that, whether the transplanted neural stem cell line was derived from the hippocampus or the olfactory bulb, the blood sugar levels gradually decreased, indicating that the diabetes was alleviated. In contrast, the diabetic rat group that did not undergo neural stem cell transplantation suffered marked deterioration in the disease state and died after eight weeks (* in Fig. 2). In addition, when the transplanted neural stem cells were removed from the alleviated diabetic rats (the broken-line arrow in Fig.2), the blood sugar level again increased.
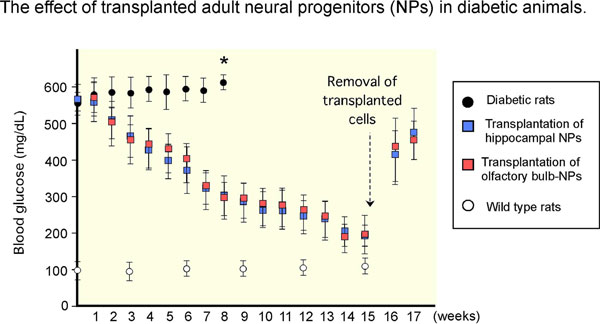 |
Figure 2 : Therapeutic efficacy of transplantation into diabetic rats of adult neural stem cells derived from diabetic rats
and effects of removal of transplanted cells (after sixteen weeks) |
An investigation was carried out using antibody stains to determine which cells produce insulin in the diabetic rat pancreas fifteen weeks after the transplantation of adult neural stem cells. In order to distinguish the transplanted adult neural stem cells from the original cells of the diabetic rats, the transplanted cells were prepared to express a green fluorescent protein as a marker. It was confirmed that almost no insulin was produced in the islets of Langerhans of the diabetic rats, whereas the transplanted neural stem cells (the green cells in Fig. 3) were effective insulin-producers.
These results indicate that diabetes was alleviated by intrapancreatic insulin production when neural stem cells derived from the hippocampi or the olfactory bulbs of diabetic rats were transplanted.
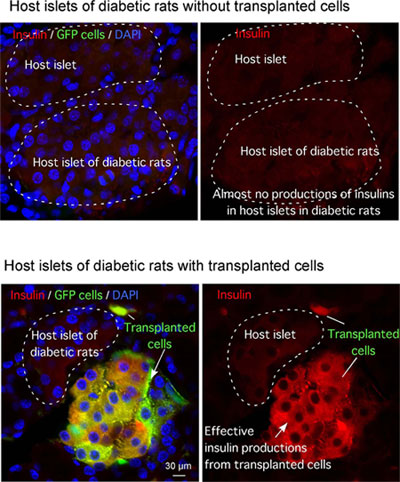 |
Figure 3 : Insulin production by transplanted adult neural stem cells
(green: transplanted olfactory-bulb-derived neural stem cells; red: insulin) |
Since the developed method is based on transplantation of autologous cells (adult stem cells from the olfactory bulb), there are no donor problems and no concerns about the adverse effects of immunosuppressive agents and it would lead to more natural regenerative therapy. The insulin-producing cells are continuously replenished by adult neural stem cells and therapeutic efficacy is thus maintained. Another advantage is that the treatment has a low carcinogenesis risk and is very safe because the treatment involves no gene transfer. This method could be used as a preliminary treatment during the stage before the onset of serious complications (retinopathy and nephropathy) and could be applied to a wide range of indications.
Based on data obtained by analysis of the mechanism of insulin production by adult neural stem cells, research and development will be carried out on the effects on neurons themselves and on the search of activating agents for more effective insulin production.